AI in Medical Coding Market Size, Share & Trends Analysis Report By Mode (In-house, Outsourced), By End User (Healthcare providers, Medical billing companies, Payers) and By Region (North America, Europe, APAC, Middle East and Africa, LATAM) Forecasts, 2026-2034
AI in Medical Coding Market Overview
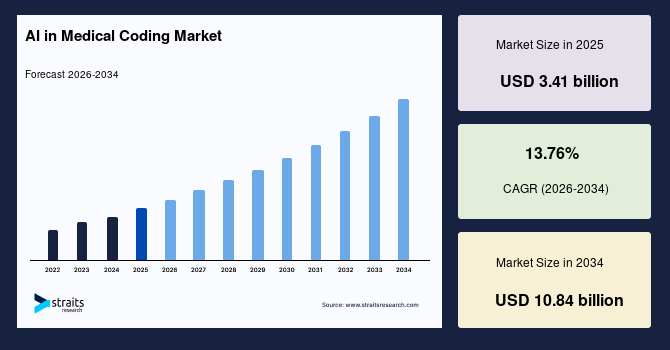
The global AI in medical coding market size is valued at USD 3.41 billion in 2025 and is estimated to reach USD 10.84 billion by 2034, growing at a CAGR of 13.76% during 2026-2034. The market observed impressive growth, stimulated by rising adoption of AI-driven workflows aimed at reducing billing errors and strengthening human oversight, as highlighted in the MedTech Intelligence feature on AI and human oversight in medical billing accuracy, which reported reductions in claim rejections by up to 40% and decreases in billing cycle time by 20–30% in early adopter health systems. This growth was closely linked to persistent challenges within medical billing.
For example, as per the report of Innovative Publishing Co., Inc., nearly half of insured Americans had reported receiving unexpected medical bills or charges for services that should have been covered, indicating systemic inefficiencies across reimbursement workflows. Medical billing errors were estimated to cost Americans approximately USD 210 billion annually and contributed to nearly USD 68 billion in avoidable healthcare expenses, intensifying financial strain on patients and providers alike. The complexity of billing processes further compounded these issues, as consumers often remained unaware that disputed charges could be challenged, creating confusion around financial responsibility and weakening confidence in the overall care and payment ecosystem.
Key Market Trends & Insights
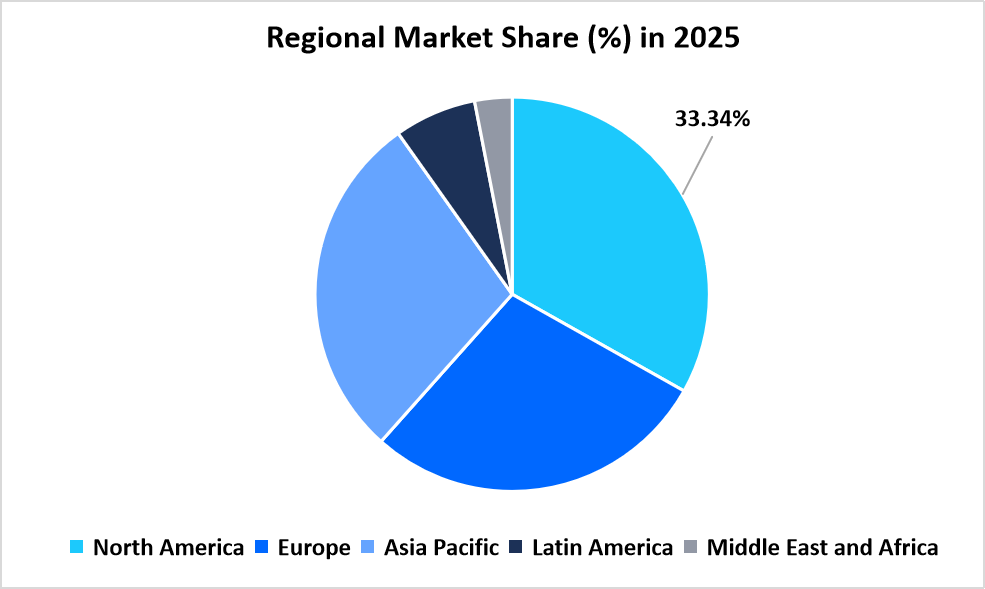
- North America held a dominant share of the global market, accounting for 33.34% in 2025.
- The Asia Pacific region is estimated to grow at the fastest pace, with a CAGR of 15.76% during the forecast period.
- Based on Mode, the in-house segment is anticipated to register the fastest CAGR of 14.87% during the forecast period.
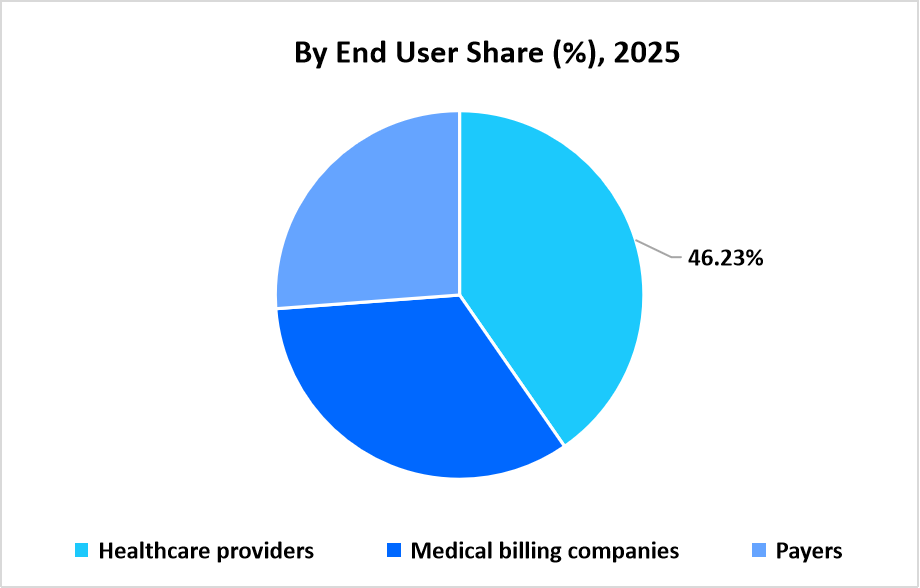
- Based on End User, the healthcare providers segment dominated the market with a revenue share of 46.23% in 2025.
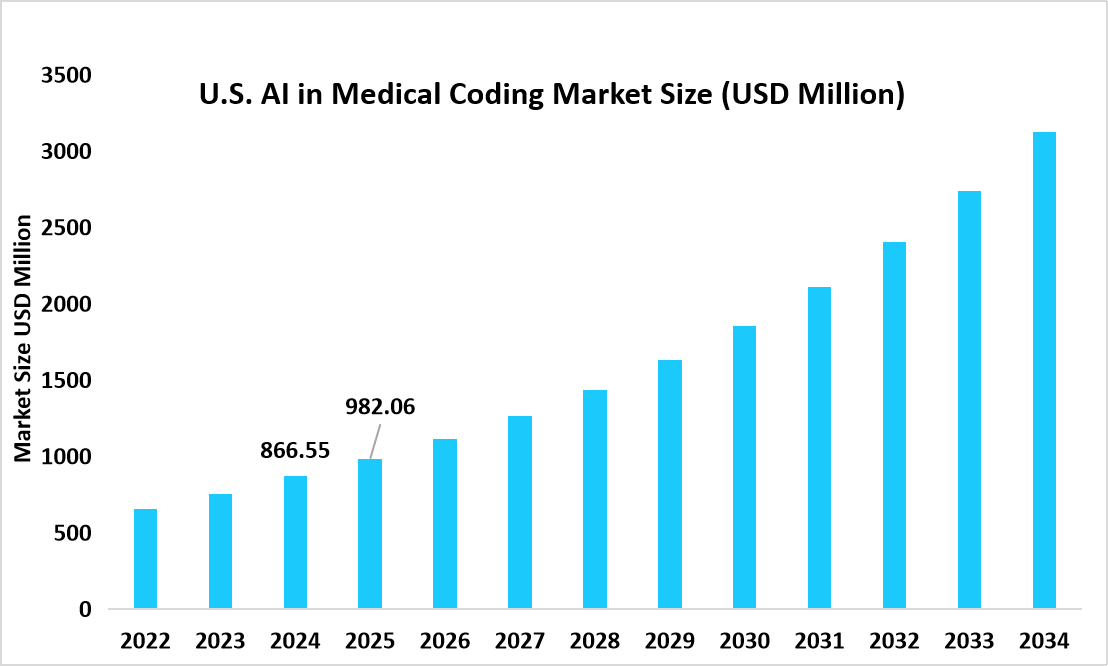
- The U.S. dominates the AI in medical coding market, valued at USD 866.55 million in 2024 and reaching USD 982.06 million in 2025.
Source: Straits Research
Market Size & Forecast
- 2025 Market Size: USD 3.41 billion
- 2034 Projected Market Size: USD 10.84 billion
- CAGR (2026-2034): 13.76%
- Dominating Region: North America
- Fastest Growing Region: Asia Pacific
The AI in medical coding market refers to the deployment of artificial intelligence technologies to automate and augment the translation of clinical documentation into standardized medical codes used for billing, reimbursement, and reporting. These solutions apply advanced language processing and contextual analysis to interpret physician notes, discharge summaries, and procedure records across inpatient and outpatient settings. The market supports both in-house and outsourced modes, allowing organizations to either deploy AI coding engines within internal systems or access them through external service providers. Adoption spans healthcare providers, medical billing companies, and payers, each leveraging AI-driven coding to improve workflow efficiency, manage documentation complexity, and support scalable revenue cycle operations within regulated healthcare environments.
Market Trends
Shift From Human-Assisted Computer-Aided Coding To Fully Autonomous Clinical Language Interpretation
The AI in medical coding market is undergoing a shift from human-assisted computer-aided coding toward fully autonomous clinical language interpretation, as providers seek to reduce dependence on manual coder review. Earlier AI tools functioned as suggestion engines that required coder confirmation, whereas current platforms process entire clinical narratives and derive codes independently. This transition supports enterprise-scale deployment across inpatient and outpatient settings, enabling consistent interpretation of physician documentation and reducing operational variability across departments.
Shift From Batch-Based Post-Encounter Coding To Continuous Documentation-Driven Coding Workflows
The market is shifting from batch-based coding performed after patient discharge to continuous coding aligned with real-time clinical documentation. AI systems are increasingly embedded within electronic health record workflows, allowing documentation to be interpreted as it is created rather than after chart completion. This shift improves coding cycle time, supports faster downstream billing workflows, and aligns coding operations more closely with clinical activity rather than administrative backlogs.
Market Summary
| Market Metric | Details & Data (2025-2034) |
|---|---|
| 2025 Market Valuation | USD 3.41 billion |
| Estimated 2026 Value | USD 3.86 billion |
| Projected 2034 Value | USD 10.84 billion |
| CAGR (2026-2034) | 13.76% |
| Dominant Region | North America |
| Fastest Growing Region | Asia Pacific |
| Key Market Players | 3M, Optum, Inc., CodaMetrix, Inc., Fathom Health, Inc., Nym Health Ltd. |
to learn more about this report Download Free Sample Report
Market Driver
Hospital Led Adoption of Autonomous Coding To Improve Revenue Cycle Throughput And Scalability
Growing pressure to improve revenue cycle throughput while managing rising clinical documentation volumes is driving hospital-led adoption of autonomous AI coding platforms. In 2024, CodaMetrix, Inc. announced expanded use of its autonomous coding platform across large multi-hospital health systems. These deployments focused on high-volume inpatient and specialty encounters, where automation supports faster chart finalization and consistent coding logic across facilities. The expansion reflected how providers increasingly prioritize AI solutions that operate directly within existing clinical workflows and scale across enterprise environments without proportional increases in coding staff.
Market Restraint
Dependence On High Quality Clinical Documentation And Structured Data Consistency
A key restraint in the AI in medical coding market is the continued dependence on high-quality and well-structured clinical documentation. Variation in physician note formats, specialty-specific terminology, and levels of documentation completeness influences how accurately AI systems interpret clinical records. As a result, organizations with fragmented documentation practices experience longer validation timelines and slower adoption, as coding outputs require additional review until documentation becomes standardized across service lines.
Market Opportunity
Integration of Autonomous Coding With Clinical Documentation Improvement And Quality Reporting
The growing integration of AI medical coding with clinical documentation improvement and quality reporting platforms presents a strong opportunity for market expansion. As healthcare organizations align documentation, coding, and performance measurement within unified workflows, AI engines extend beyond code assignment into documentation optimization and reporting support. This integration strengthens demand for platforms that connect clinical narratives with reimbursement logic and performance tracking, positioning AI medical coding as a core infrastructure component within modern digital health operations rather than a standalone automation tool.
Regional Analysis
North America dominated the market for AI in medical coding with share of 33.34%, supported by early adoption of electronic health records and standardized reimbursement systems. Hospitals and health systems increasingly deploy AI driven coding engines to manage rising documentation volumes, specialty level coding complexity, and payer compliance requirements. Integration of AI coding directly within clinical and billing workflows supports faster claim readiness and operational scalability.
In the U.S., adoption is reinforced by national coding and billing standards administered by Centers for Medicare and Medicaid Services, which mandate structured ICD and CPT based reporting for reimbursement. Health systems across multiple states implemented autonomous and AI assisted coding solutions within Epic environments to accelerate inpatient and outpatient coding while maintaining alignment with federal billing rules. These deployments position the U.S. as a reference market for enterprise scale AI medical coding adoption.
Asia Pacific AI in Medical Coding Market Insights
Asia Pacific is emerging as a fastest growth market with CAGR of 15.76% driven by rapid hospital digitalization and expansion of private healthcare networks. AI medical coding solutions are deployed to support multi payer billing environments, cross border patient care, and high throughput clinical operations. Adoption remains concentrated within large hospital groups and specialty centers.
In India, private tertiary care hospitals apply AI driven coding platforms to manage complex insurance claims, international patient billing, and specialty procedures across multisite networks. These deployments support operational efficiency in environments characterized by high patient volumes and diverse payer structures.
Source: Straits Research
Europe Market Insights
Europe market is shaped by centralized healthcare systems and diagnosis-related group-based reimbursement models. AI in medical coding is primarily adopted to standardize documentation quality and reduce variability across hospital networks rather than fully replace human coders. Regulatory oversight and audit driven reimbursement structures influence gradual but consistent adoption.
In the UK, National Health Service hospitals increasingly use AI assisted coding tools to support clinical coding teams managing high admission volumes and complex case mix adjustments. AI platforms focus on interpreting clinician narratives and aligning outputs with NHS coding standards, enabling improved consistency across trusts while supporting workforce efficiency within publicly funded healthcare systems.
Latin America Market Insights
Latin America market is influenced by gradual modernization of hospital information systems and selective private sector investment. AI in medical coding is primarily used within large private hospital groups that manage insured and international patient populations.
In Brazil, leading private hospitals deploy AI assisted coding tools to standardize clinical documentation across multispecialty facilities and support accurate billing within mixed public and private reimbursement frameworks. Adoption remains focused on urban centers with advanced digital infrastructure.
Middle East and Africa Market Insights
The Middle East and Africa region exhibits emerging adoption aligned with national healthcare digital transformation programs and hospital automation initiatives. AI medical coding is implemented as part of broader revenue cycle modernization rather than as a standalone solution.
In the United Arab Emirates, hospital networks integrate AI based coding within centralized health information platforms to support standardized billing and regulatory compliance across emirates. In South Africa, private hospital groups apply AI assisted coding to harmonize documentation and billing practices across multisite operations, reflecting gradual regional market development.
Mode Insights
The outsourced mode dominated the market in 2025, supported by strong dependence on specialized vendors that deliver AI-driven medical coding through managed services and cloud-based platforms. Healthcare organizations increasingly rely on outsourced models to manage coder shortages, variable claim volumes, and compliance-intensive coding requirements. Companies such as AGS Health, LLC, and nThrive, Inc. operate large-scale AI-enabled coding operations that support hospitals and physician groups across multiple specialties. Outsourced dominance is reinforced by centralized model training, faster implementation cycles, and reduced internal infrastructure burden.
The in-house mode is the fastest growing, expanding at 14.87%, driven by health systems investing directly in internal AI coding platforms integrated within their electronic health record environments. Large provider networks adopt in-house models to retain control over clinical data, customize specialty-specific coding workflows, and align automation with internal compliance governance. Vendors such as CodaMetrix, Inc. support this trend by enabling autonomous coding deployments within provider-managed systems rather than service-based outsourcing arrangements.
End User Insights
The healthcare providers segment dominated the market in 2025 with a share of 46.23%, reflecting direct adoption of AI medical coding across hospitals, integrated delivery networks, and multispecialty clinics. Providers deploy AI-driven coding to accelerate chart completion, reduce discharged not final billed timelines, and standardize coding outputs across departments. Health systems using solutions from Nym Health Ltd. and 3M Company reinforce provider-led dominance through inpatient and outpatient coding automation.
The payers segment is the fastest-growing end user, recording 14.23%, as insurers increasingly adopt AI medical coding to strengthen claims validation and reimbursement governance. Payers apply AI models to cross-verify submitted codes against clinical documentation and coverage policies, supporting faster adjudication and reduced post-payment reviews. This growth reflects expanding insurer focus on automation-driven claims processing and coding consistency across provider networks.
Source: Straits Research
Competitive Landscape
The global AI in medical coding market reflects moderate consolidation, characterized by the presence of healthcare IT vendors, revenue cycle management solution providers, and specialized artificial intelligence software companies.
-
Nym Health Ltd.: An Emerging Market Player
Nym Health Ltd. represents an emerging and specialized participant within the AI in medical coding industry, with a concentrated focus on fully autonomous medical coding across inpatient and outpatient encounters. The company differentiates itself through a proprietary clinical language understanding architecture that interprets unstructured physician documentation and converts it into compliant billing codes without rule-based human intervention.
- In August 2024, Nym Health Ltd., a provider of autonomous medical coding solutions, announced that its medical coding engine received Toolbox designation within the Fully Autonomous Coding category of Epic’s Showroom. The Toolbox program included third-party applications that aligned with Epic's recommended connection practices for defined functionality categories, strengthening enterprise-level adoption within the market.
List of Key and Emerging Players in AI in Medical Coding Market
- 3M
- Optum, Inc.
- CodaMetrix, Inc.
- Fathom Health, Inc.
- Nym Health Ltd.
- Dolbey Systems, Inc.
- nThrive, Inc.
- AGS Health, LLC
- XpertDox, Inc.
- HealthOrbit AI, Inc.
- AdvancedMD, Inc.
- RapidClaims AI, Inc.
- Sully.ai, Inc.
- TachyHealth Group
- Others
Recent Developments
- October 2025: Suki, an AI-based healthcare company, expanded its assisted revenue cycle capabilities to provide more specific automation and generate additional codes, including CPT and E/M codes.
- May 2025: Ambience Healthcare announced a new medical coding that it trained using OpenAI's reinforcement fine-tuning technology, which outperforms doctors by 27%.
Report Scope
| Report Metric | Details |
|---|---|
| Market Size in 2025 | USD 3.41 billion |
| Market Size in 2026 | USD 3.86 billion |
| Market Size in 2034 | USD 10.84 billion |
| CAGR | 13.76% (2026-2034) |
| Base Year for Estimation | 2025 |
| Historical Data | 2022-2024 |
| Forecast Period | 2026-2034 |
| Report Coverage | Revenue Forecast, Competitive Landscape, Growth Factors, Environment & Regulatory Landscape and Trends |
| Segments Covered | By Mode, By End User |
| Geographies Covered | North America, Europe, APAC, Middle East and Africa, LATAM |
| Countries Covered | US, Canada, UK, Germany, France, Spain, Italy, Russia, Nordic, Benelux, China, Korea, Japan, India, Australia, Taiwan, South East Asia, UAE, Turkey, Saudi Arabia, South Africa, Egypt, Nigeria, Brazil, Mexico, Argentina, Chile, Colombia |
to learn more about this report Download Free Sample Report
AI in Medical Coding Market Segments
By Mode
- In-house
- Outsourced
By End User
- Healthcare providers
- Medical billing companies
- Payers
By Region
- North America
- Europe
- APAC
- Middle East and Africa
- LATAM
Frequently Asked Questions (FAQs)
Debashree Bora
Healthcare Lead
Debashree Bora is a Healthcare Lead with over 7 years of industry experience, specializing in Healthcare IT. She provides comprehensive market insights on digital health, electronic medical records, telehealth, and healthcare analytics. Debashree’s research supports organizations in adopting technology-driven healthcare solutions, improving patient care, and achieving operational efficiency in a rapidly transforming healthcare ecosystem.










































