Antibiotic Resistance Market Size, Share & Trends Analysis Report By Disease (cUTI (Complicated Urinary Tract Infections), CDI (Clostridioides difficile Infection), ABSSSI (Acute bacterial skin and skin structure infections), HABP (Hospital-acquired bacterial pneumonia), CABP (Community-acquired pneumonia), cIAI (Complicated intra-abdominal infection), BSI (Bloodstream infection)), By Pathogen (coli, pneumoniae, aeruginosa, aureus, baumannii, influenzae, difficile, faecium), By Drug Class (Oxazolidinones, Lipoglycopeptides, Tetracyclines, Combination therapies, Cephalosporins, Others), By Mechanism of Action (Protein Synthesis Inhibitors, Cell Wall Synthesis Inhibitors, RNA Synthesis Inhibitors, DNA Synthesis Inhibitors, Others), By Distribution Channel (Hospital Pharmacies, Retail Pharmacies, Online Pharmacies) and By Region (North America, Europe, APAC, Middle East and Africa, LATAM) Forecasts, 2026-2034
Antibiotic Resistance Market Overview
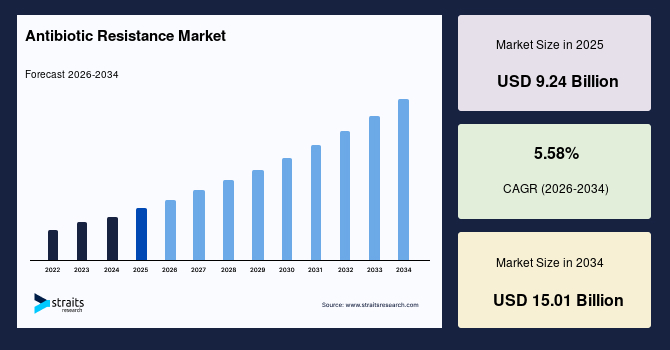
The global antibiotic resistance market size is estimated at USD 9.24 billion in 2025 and is projected to reach USD 15.01 billion by 2034, growing at a CAGR of 5.58% during the forecast period. Sustained growth of the market is propelled by rising global focus on resistant bacterial infections and expanding adoption of targeted antimicrobial therapies across multiple disease categories.
Key Market Trends & Insights
- North America held a dominant share of the global market, accounting for 41.13%.
- The Asia Pacific region is growing at the fastest pace, with a CAGR of 7.58%.
- By Disease, the cUTI (Complicated Urinary Tract Infections) segment dominated the market in 2025 with a share of 27.45%.
- By Pathogen, K. pneumoniae segment dominated the market with a share of 32.34%.
- By Drug Class, the Oxazolidinones segment dominated the market in 2025 with a share of 36.78%.
- By Mechanism of Action, the Cell Wall Synthesis Inhibitors segment dominated the market with a share of 25.87%.
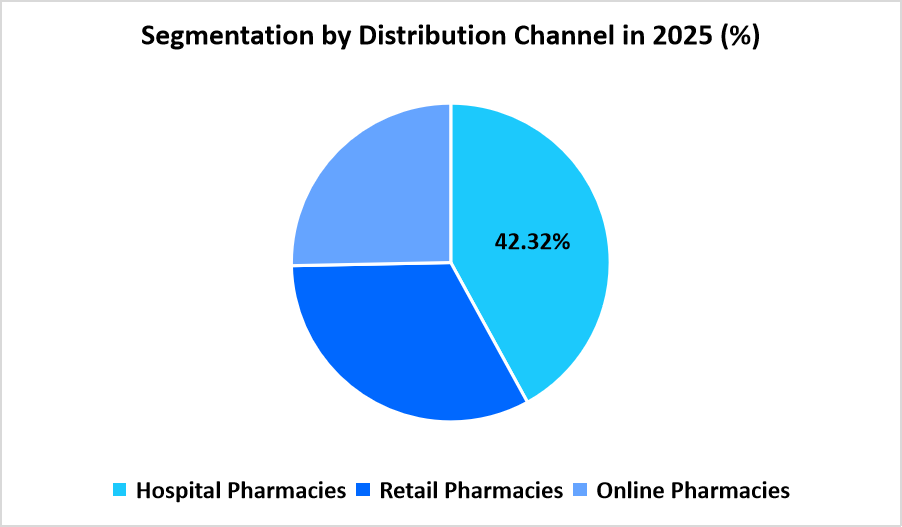
- By Distribution Channel, the Hospital pharmacies segment dominated the market in 2025 with a share of 42.32%.
- The U.S. dominates the global antibiotic resistance market, valued at USD 3.27 billion in 2024 and reaching USD 3.43 billion in 2025.
Graph: U.S. Market Revenue Forecast (2022 – 2034)
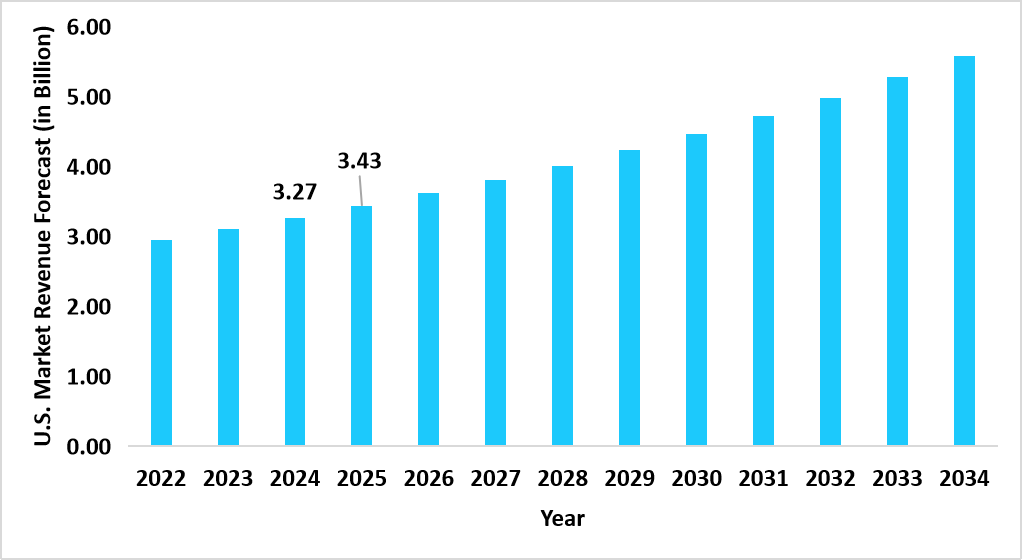
Source: Straits Research
Market Size & Forecast
- 2025 Market Size: USD 9.24 billion
- 2034 Projected Market Size: USD 15.01 billion
- CAGR (2025 to 2034): 5.58%
- Dominating Region: North America
- Fastest Growing Region: Asia Pacific
The global antibiotic resistance market encompasses a broad spectrum of therapeutic, diagnostic, and distribution activities centered on managing infections that no longer respond to standard antimicrobial agents. The market includes treatments for disease categories such as complicated urinary tract infections, Clostridioides difficile infection, acute bacterial skin and skin structure infections, hospital acquired and community acquired pneumonia, complicated intra-abdominal infections, and bloodstream infections. It spans pathogens that frequently demonstrate rising resistance patterns, including E. coli, K. pneumoniae, P. aeruginosa, S. aureus, A. baumannii, S. pneumoniae, H. influenzae, C. difficile, and E. faecium. The market covers multiple drug classes such as oxazolidinones, lipoglycopeptides, tetracyclines, combination therapies, cephalosporins, and other antibacterial agents, each targeting specific resistance pathways. It is further defined by mechanisms of action that include protein synthesis inhibitors, cell wall synthesis inhibitors, RNA synthesis inhibitors, DNA synthesis inhibitors, and other antimicrobial approaches. Distribution occurs primarily through hospital pharmacies for acute cases, retail pharmacies for outpatient treatment courses, and online pharmacies for digitally managed antibiotic dispensing, creating a comprehensive ecosystem responding to the global rise of resistant bacterial infections.
Latest Market Trends
Rising Interest in Bacteriophage Inclusion in Clinical Protocols
A growing trend in the antibiotic resistance market is the gradual inclusion of bacteriophage-based approaches within clinical discussions for therapy planning. Clinicians and research groups are assessing phage libraries to match strain-specific profiles, allowing targeted neutralization of bacterial colonies. As phage collections expand within research networks, healthcare systems are exploring structured pathways for their controlled use in difficult-to-treat infections.
Expansion of Localized Antimicrobial Stewardship Cells in Large Hospitals
The major trend is the creation of stewardship cells within large hospitals where dedicated teams monitor antibiotic selection patterns across departments. These units assess ward-level usage, conduct seasonal audits, and coordinate advisory sessions with prescribing teams. This approach is shaping more disciplined antibiotic routing across hospitals and refining consumption patterns in high-volume care units.
Market Summary
| Market Metric | Details & Data (2025-2034) |
|---|---|
| 2025 Market Valuation | USD 9.24 Billion |
| Estimated 2026 Value | USD 9.72 Billion |
| Projected 2034 Value | USD 15.01 Billion |
| CAGR (2026-2034) | 5.58% |
| Dominant Region | North America |
| Fastest Growing Region | Asia-Pacific |
| Key Market Players | Sanofi, Pfizer Inc., Merck & Co., Inc., GSK plc., Abbott |
to learn more about this report Download Free Sample Report
Antibiotic Resistance Market Driver
Rising Use of Genomic Sequencing for Pathogen Mapping
A major driver for the market is the rising incorporation of genomic sequencing for pathogen mapping. Hospitals and research centers are conducting sequence based studies to track mutation pathways, enabling clinicians to adjust therapy choices with greater precision. As sequencing platforms grow across reference laboratories, therapy alignment with genetic signatures is becoming more structured.
Market Restraint
Growing Caution Toward Escalation Therapy in Recurrent Infections
A restraint for the market is growing caution toward escalation therapy for patients presenting recurrent infections. Physicians are reviewing previous antibiotic cycles closely to reduce repeated exposure, which results in slower transition to higher-tier agents. This cautious approach limits prescription volume for advanced drug classes in routine cases.
Market Opportunity
Expansion of Regional Bioinnovation Hubs Focused on Resistant Pathogens
A strong opportunity arises from the formation of regional bioinnovation hubs dedicated to resistant pathogen research. These hubs bring together microbiology units, academic centers, and start-ups to co-develop screening tools and preliminary drug candidates. As these hubs widen their collaborations, they create fresh pathways for antimicrobial development and open new directions for commercial growth.
Regional Analysis
North America held a substantial share of 41.13% in the antibiotic resistance market in 2025 due to the rapid uptake of antimicrobial stewardship practices across hospitals and outpatient centers. Growth in this region arose from structured reimbursement pathways for infectious disease care, along with steady expansion of susceptibility testing across clinical laboratories. Pharmaceutical companies in the United States and Canada supported broad distribution of antibacterial therapies and diagnostics across retail outlets, specialty clinics, and digital pharmacy platforms.
The U.S. market expanded as federal-level initiatives improved surveillance for resistant infections, which encouraged consistent use of diagnostic-guided treatments across healthcare facilities. These initiatives promoted wider circulation of priority antimicrobial agents within both public and private hospitals, raising overall therapy utilization.
Asia Pacific Market Insights
Asia Pacific recorded the fastest CAGR of 7.58% during the forecast period due to rising awareness of community-level infection control and wider integration of antimicrobial treatment pathways across emerging economies. Countries in East and South Asia introduced expanded pathogen detection programs that increased early case identification and supported larger volumes of antibiotic prescriptions for targeted conditions. Pharmaceutical firms and academic centers across the region advanced multiple clinical studies and supported technology upgrades in laboratory networks to address growing patient volumes.
Growth in India is shaped by national digital health schemes that enable real-time monitoring of antibiotic dispensing across government-supported hospitals. These schemes improved drug allocation in district-level facilities, which strengthened supply consistency and raised market adoption through public healthcare channels.
Pie Chart: Regional Market Share, 2025
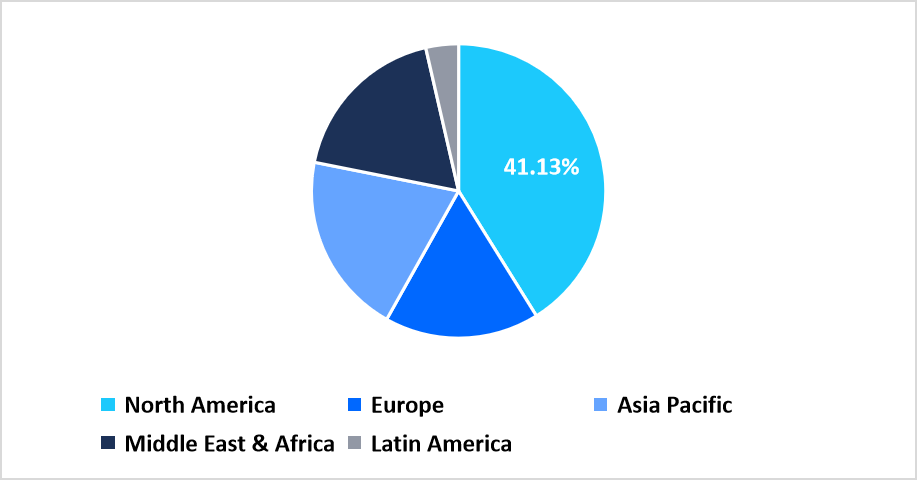
Source: Straits Research
Europe Market Insights
Europe registered stable advancement as healthcare regulators promoted structured infection prevention frameworks within primary care and long-term care centers. These frameworks encouraged more frequent clinician consultations and increased demand for validated antibiotic classes used for controlled treatment courses. Additionally, coordinated efforts among European health agencies supported steady research activity and maintained dependable antimicrobial supply chains across member countries.
In Germany, market expansion is influenced by federal-level programs centered on routine infection awareness campaigns that encourage timely visits to clinicians. These campaigns increased patient engagement and raised prescription volumes for chronic infection management within statutory insurance networks.
Middle East and Africa Market Insights
Middle East and Africa noted rising use of antibiotics driven by national infection tracking drives conducted by government health ministries and clinical associations. Community-level screening in urban and peri-urban regions increased case reporting, which contributed to higher treatment initiation. Partnerships between public health departments and private pharmaceutical distributors improved medicine flow across national hospitals and remote treatment sites.
In Saudi Arabia, the market progressed as targeted wellness outreach programs were implemented with support from regional clinical institutions. These programs focused on early detection of infection risks among the working population, which contributed to expanded use of prescribed antimicrobials.
Latin America Market Insights
Latin America observed increasing adoption of antibiotic therapies due to broader medical outreach programs created for rural and geographically distant regions. Countries in the region introduced integrated teleconsultation systems that connected infectious disease specialists with underserved zones, which encouraged regular monitoring and follow-up visits. This drove continuous distribution of antimicrobials across both government-funded and private healthcare systems.
In Brazil, market growth is shaped by cross-state coordination that supported structured tracking of resistant infection cases. Regional health authorities supplied antibacterial drugs through mobile medical units that travelled to riverine and distant settlements, which increased access and strengthened overall market expansion.
Disease Insights
The cUTI (Complicated Urinary Tract Infections) segment dominated the market in 2025 with a share of 27.45%. Rising diagnostic confirmations of complicated urinary tract cases supported sustained prescription levels for broad-spectrum agents across outpatient and inpatient units. Consistent treatment initiation for recurrent infections further strengthened the leading position of this segment.
The CDI segment recorded the fastest rise with a growth rate of 6.12%. Increased recognition of toxin-mediated gastrointestinal infections across clinical settings encouraged wider treatment uptake. Laboratory use of stool-based assays improved case identification, contributing to the expansion of this category during the forecast period.
Pathogen Insights
The K. pneumoniae segment dominated the market with a share of 32.34%. Higher occurrence of resistant strains within intensive care wards and surgical units resulted in elevated demand for targeted antimicrobials. Hospitals adopted stricter culture based selection practices which raised utilization related to this pathogen group.
The C. difficile segment recorded the fastest progression with a growth rate of 6.34%. Greater reliance on toxin assays and molecular panels increased detection in early disease stages. This broadened the use of prescribed agents intended for controlled treatment courses, contributing to rapid market traction for this segment.
Drug Class Insights
The Oxazolidinones segment dominated the market in 2025 with a share of 36.78%. Their growing clinical preference for resistant gram positive infections supported elevated use across tertiary care centers. Physicians selected this class for complex cases, which reinforced its dominant standing through the year.
The Combination therapies segment achieved the fastest rise with a growth rate of 6.58%. Rising adoption of multi-agent regimens for high-risk infections guided stronger year-over-year expansion. Treatment plans relying on paired mechanisms encouraged broader clinical acceptance within critical care settings.
Mechanism of Action Insights
The Cell Wall Synthesis Inhibitors segment dominated the market with a share of 25.87%. Frequent use of these agents for respiratory, urinary, and surgical site infections sustained high prescription counts. Clinicians continued to prefer these therapies for structured treatment pathways, reinforcing their leadership within this category.
The RNA Synthesis Inhibitors segment recorded the fastest increase with a growth rate of 6.72%. Greater inclusion of this mechanism in revised clinical protocols expanded its utilization across select bacterial infections. Wider laboratory reporting of target organisms supported progressive market growth for this segment.
Distribution Channel Insights
The Hospital pharmacies segment dominated the market in 2025 with a share of 42.32%. Admission-related infection management increased dispensing volumes within inpatient units. Surgical departments and isolation wards continued to source sizable quantities of antimicrobials, supporting the dominance of this channel.
The Retail pharmacies segment registered the fastest expansion with a growth rate of 6.98%. Rising outpatient consultations for community-level infections encouraged steady prescription refills. Extended operating hours and wider neighbourhood presence contributed to the increasing uptake through this channel.
Source: Straits Research
Competitive Landscape
The global antibiotic resistance market is moderately fragmented, with competition spread across large pharmaceutical companies, clinical-stage biotechs focused on novel antimicrobials, generic drug manufacturers supplying essential antibiotics, and non-profit or public-private organizations accelerating R&D, stewardship, and diagnostic innovation.
Venatorx Pharmaceuticals, Inc.: An emerging market player
Venatorx Pharmaceuticals, Inc. emerged as a strong player in the global market, concentrating on the development of novel broad-spectrum antibiotics and β-lactamase inhibitors targeting multidrug-resistant Gram-negative pathogens.
- In 2025, Venatorx Pharmaceuticals, Inc. advanced its next-generation antimicrobial candidates through late-stage clinical milestones, strengthening its position as an innovation-driven biotech delivering differentiated mechanisms capable of addressing some of the most severe and treatment-resistant bacterial infections.
List of Key and Emerging Players in Antibiotic Resistance Market
- Sanofi
- Pfizer Inc.
- Merck & Co., Inc.
- GSK plc.
- Abbott
- Johnson & Johnson
- Novartis AG
- Bayer AG
- Shionogi & Co., Ltd.
- Acurx Pharmaceuticals, Inc.
- Melinta Therapeutics LLC
- Paratek Pharmaceuticals, Inc.
- VenatoRx Pharmaceuticals, Inc.
- Spero Therapeutics
- Summit Therapeutics Inc.
- Theravance Biopharma.
- Wockhardt
- Zai Lab
- Xellia Pharmaceuticals
- Others
Strategic Initiatives
- November 2025: The Government of Sweden adopted a new 10-year national strategy to combat Antimicrobial Resistance (AMR). The strategy included 17 overarching quantifiable, time-bound goals across five focus areas, including preventive measures, responsible antibiotic use, improved access to diagnostics and medicines, enhanced surveillance in human and animal health, and environmental considerations, making it a landmark regulatory commitment that reinforces efforts to curb antibiotic resistance globally.
- November 2025: A grant proposal titled “Combatting Antimicrobial Resistance Through Community Labs” outlined a project aimed at reducing AMR in underserved communities by establishing community-level diagnostic labs. The proposal focused on setting up pilot labs for basic diagnostic tests, training community health workers, implementing local antibiotic stewardship programs, raising awareness among thousands of people, and building a community-based AMR data monitoring system to track resistance trends.
Report Scope
| Report Metric | Details |
|---|---|
| Market Size in 2025 | USD 9.24 Billion |
| Market Size in 2026 | USD 9.72 Billion |
| Market Size in 2034 | USD 15.01 Billion |
| CAGR | 5.58% (2026-2034) |
| Base Year for Estimation | 2025 |
| Historical Data | 2022-2024 |
| Forecast Period | 2026-2034 |
| Report Coverage | Revenue Forecast, Competitive Landscape, Growth Factors, Environment & Regulatory Landscape and Trends |
| Segments Covered | By Disease, By Pathogen, By Drug Class, By Mechanism of Action, By Distribution Channel |
| Geographies Covered | North America, Europe, APAC, Middle East and Africa, LATAM |
| Countries Covered | US, Canada, UK, Germany, France, Spain, Italy, Russia, Nordic, Benelux, China, Korea, Japan, India, Australia, Taiwan, South East Asia, UAE, Turkey, Saudi Arabia, South Africa, Egypt, Nigeria, Brazil, Mexico, Argentina, Chile, Colombia |
to learn more about this report Download Free Sample Report
Antibiotic Resistance Market Segments
By Disease
- cUTI (Complicated Urinary Tract Infections)
- CDI (Clostridioides difficile Infection)
- ABSSSI (Acute bacterial skin and skin structure infections)
- HABP (Hospital-acquired bacterial pneumonia)
- CABP (Community-acquired pneumonia)
- cIAI (Complicated intra-abdominal infection)
- BSI (Bloodstream infection)
By Pathogen
- coli
- pneumoniae
- aeruginosa
- aureus
- baumannii
- influenzae
- difficile
- faecium
By Drug Class
- Oxazolidinones
- Lipoglycopeptides
- Tetracyclines
- Combination therapies
- Cephalosporins
- Others
By Mechanism of Action
- Protein Synthesis Inhibitors
- Cell Wall Synthesis Inhibitors
- RNA Synthesis Inhibitors
- DNA Synthesis Inhibitors
- Others
By Distribution Channel
- Hospital Pharmacies
- Retail Pharmacies
- Online Pharmacies
By Region
- North America
- Europe
- APAC
- Middle East and Africa
- LATAM
Frequently Asked Questions (FAQs)
Debashree Bora
Healthcare Lead
Debashree Bora is a Healthcare Lead with over 7 years of industry experience, specializing in Healthcare IT. She provides comprehensive market insights on digital health, electronic medical records, telehealth, and healthcare analytics. Debashree’s research supports organizations in adopting technology-driven healthcare solutions, improving patient care, and achieving operational efficiency in a rapidly transforming healthcare ecosystem.










































