Healthcare Reimbursement Market Size, Share & Trends Analysis Report By Claim (Full Reimbursement, Partial Reimbursement), By Payer (Public Payers, Private Payers), By Service Provider (Hospitals, Specialty Clinics, Diagnostics Laboratory, Ambulatory Surgery Center) and By Region (North America, Europe, APAC, Middle East and Africa, LATAM) Forecasts, 2025-2033
Healthcare Reimbursement Market Size
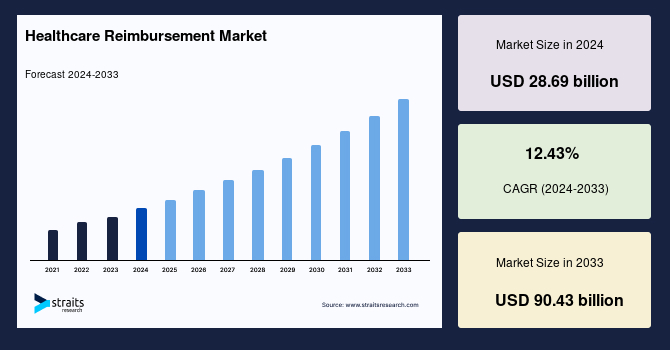
The global healthcare reimbursement market size was valued at USD 28.69 billion in 2024 and is projected to grow from USD 35.55 billion in 2025 to reach USD 90.43 billion by 2033, exhibiting a CAGR of 12.43% during the forecast period (2025-2033).
Healthcare reimbursement refers to the process by which healthcare providers receive payment for the services they deliver to patients. These payments can come from various sources, including insurance companies, government programs (like Medicare or Medicaid), and patients themselves. The reimbursement process involves submitting claims for services provided, which are then reviewed and processed based on established rates, policies, and coverage details.
The market is experiencing significant growth, fueled by evolving payment models, expanding healthcare access, and a rising demand for cost-effective treatment solutions. Both governments and private insurers are restructuring reimbursement policies to better accommodate advanced treatments such as digital health services, precision medicine, and innovative drug therapies. One of the most notable shifts is the move toward value-based care, which prioritizes patient outcomes over the volume of services provided, ultimately reshaping reimbursement frameworks on a global scale.
Technological advancements, particularly AI-driven claims processing and blockchain-based medical billing, are playing a pivotal role in streamlining reimbursement operations. These innovations are reducing fraud, enhancing efficiency, and driving operational cost savings, thereby improving the overall reimbursement process. Alongside this, the increasing prevalence of chronic diseases is contributing to the expansion of both public and private health insurance programs, further driving demand for reimbursement solutions.
Opportunities for market expansion are emerging through cross-border health insurance solutions, strategic partnerships between insurers and healthcare providers, and the integration of remote patient monitoring into reimbursement policies.
- For example, in October 2024, Prudential Hong Kong Limited entered into a strategic partnership with Guangzhou United Family Hospital (GZU) and Shanghai United Family Hospital (SHU), becoming the first Hong Kong-based insurer to collaborate with both facilities simultaneously.
This partnership enables Prudential customers to access Medical Expenses Direct Billing Services at these hospitals, enhancing cross-border healthcare options and ensuring seamless medical coverage for policyholders. Such partnerships highlight the growing focus on cross-border health insurance solutions, improving accessibility and financial ease for policyholders seeking quality medical care outside their home country.
Latest Market Trends
Growth of Remote Patient Monitoring Reimbursement
The adoption of digital health solutions is driving a significant expansion in the reimbursement for Remote Patient Monitoring (RPM) globally. Governments and private insurers are increasingly updating policies to include home-based monitoring for chronic conditions such as diabetes, hypertension, and heart disease.
- For example, in November 2023, the Centers for Medicare & Medicaid Services (CMS) expanded RPM reimbursement to include Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs). These facilities are now able to bill for RPM services under the general care management code HCPCS G0511, improving access to remote monitoring for underserved populations.
This policy change underscores the growing recognition of RPM’s role in managing chronic conditions and reducing healthcare disparities.
Expanding Coverage for Personalized Medicine
The growing adoption of precision medicine is prompting insurers and government programs to expand reimbursement for genomic testing, targeted therapies, and biomarker-driven treatments. This shift is enhancing disease prediction, prevention, and the development of customized treatment plans, particularly for cancer and rare diseases.
- In January 2024, Medicare expanded reimbursement for Next-Generation Sequencing (NGS) in oncology, providing greater access to genomic testing for patients with advanced cancers, including prostate, ovarian, and breast cancer. This expansion supports earlier detection, personalized treatment options, and better patient outcomes.
Therefore, it reflects the increasing value placed on precision medicine, which is driving growth in the reimbursement market by offering more effective, patient-centered care.
Market Summary
| Market Metric | Details & Data (2024-2033) |
|---|---|
| 2024 Market Valuation | USD 28.69 Billion |
| Estimated 2025 Value | USD 35.55 Billion |
| Projected 2033 Value | USD 90.43 Billion |
| CAGR (2025-2033) | 12.43% |
| Dominant Region | North America |
| Fastest Growing Region | Asia Pacific |
| Key Market Players | UNITEDHEALTH GROUP, Aviva, Allianz Care, CVS Health, BNP Paribas |
to learn more about this report Download Free Sample Report
Healthcare Reimbursement Market Driving Factors
Increasing Healthcare Expenditures and Insurance Penetration
Rising healthcare costs and expanding insurance coverage are key factors fueling the demand for efficient reimbursement systems. Governments and private insurers are increasing healthcare spending to improve accessibility, affordability, and financial protection, particularly in emerging markets.
- For instance, in August 2024, India’s National Health Authority (NHA) launched the National Health Claims Exchange (NHCX) to streamline insurance claims processing. This platform standardizes health claims data exchange, enhancing transparency, improving efficiency, and speeding up settlements while reducing operational costs.
Such initiatives reflect a growing focus on improving reimbursement systems to ensure equitable healthcare access, helping to reduce financial barriers and ensure timely medical care for an expanding insured population.
Market Restraining Factors
Limited Coverage for Advanced and Experimental Treatments
One of the key challenges in the market is the limited coverage of advanced and experimental treatments. Reimbursement policies frequently exclude or only partially cover high-cost, cutting-edge therapies such as gene therapy, CAR-T cell therapy, and personalized medicine. These treatments face strict approval criteria from insurers due to their high costs, uncertain long-term outcomes, and complex approval processes. This hesitation from payers leads to delayed adoption and increased out-of-pocket expenses for patients, or they are left to rely on clinical trials. Consequently, this restricts the widespread accessibility and integration of breakthrough medical innovations into standard care.
Market Opportunity
Growing Demand for Cross-Border Health Insurance
Rising medical tourism and globalization are boosting demand for cross-border health insurance, enabling patients to seek high-quality and cost-effective treatments abroad. Insurers are expanding international coverage to cater to expatriates, business travelers, and medical tourists. As healthcare systems become more interconnected, insurers are developing flexible reimbursement models to streamline claims processing and ensure seamless access to medical services across borders.
- For instance, in January 2025, GeoBlue and MetLife Worldwide Benefits collaborated to introduce Globaline, a comprehensive suite of health, life, and long-term disability products designed for expatriate employees. This partnership aims to provide seamless international coverage, meeting the rising demand for cross-border health insurance among global workers.
These developments open new opportunities in the healthcare reimbursement market by boosting demand for specialized insurance plans, fostering innovation in claims processing, and expanding insurer networks to accommodate a globally mobile population.
Regional Insights
North America: Dominant Region with 40.5% Market Share
North America maintains a dominant position in the global healthcare reimbursement market, driven by high insurance penetration and supportive government policies, including Medicare and Medicaid. The presence of major private insurers such as UnitedHealth Group and Aetna Inc. further strengthens the market as they continuously expand their reimbursement policies to cover advanced treatments. Moreover, the region’s adoption of value-based reimbursement models and advancements in telehealth reimbursement are playing a pivotal role in enhancing healthcare accessibility and driving continued market growth. These factors position North America as a key leader in the global market.
Asia Pacific: Fastest Growing Region with the Highest Market Cagr
Asia-Pacific is set to experience the fastest growth, driven by a rapidly expanding middle class, increasing medical tourism, and rising government efforts to improve universal healthcare access. Countries like India, China, and Japan are implementing comprehensive policies aimed at broadening insurance coverage and streamlining reimbursement processes. The region’s accelerated digitalization of healthcare systems, alongside expanding access to care, is creating significant opportunities for insurers and healthcare providers to enhance and modernize reimbursement models.
Countries Insights
- U.S.- The U.S. healthcare reimbursement market is leading, supported by high insurance penetration and continuous regulatory updates. In November 2024, CMS included AI-enhanced electrocardiogram (AI-ECG) technology in the 2025 Hospital Outpatient Prospective Payment System (OPPS) final rule, allowing reimbursement for cardiac assessments using AI algorithms developed by companies like Tempus and Anumana. This progressive move enhances patient access to innovative treatments, further positioning the U.S. as a market leader in integrating cutting-edge technologies into reimbursement frameworks.
- Germany- Germany remains one of Europe's largest markets, driven by universal health coverage and efficient reimbursement systems. The country continually expands reimbursement for innovative treatments, including digital health solutions. In November 2024, contextflow, a provider of AI-driven lung cancer detection, partnered with IKK Südwest through the Healthy Hub initiative to integrate AI technology into reimbursement. This highlighted Germany's commitment to advancing healthcare reimbursement, ensuring broader access to advanced diagnostic tools and innovative treatments for its population.
- UK- The UK healthcare reimbursement industry is fueled by government funding, the expansion of private insurance, and the adoption of digital health solutions. The NHS Long Term Plan focuses on value-based care, increasing reimbursement for preventive and remote healthcare services. Regulatory approvals for innovative treatments, alongside expanded insurer coverage, are contributing to market growth. The UK is positioning itself to enhance accessibility and affordability, particularly in preventive care, remote services, and advanced therapies.
- India– India's healthcare reimbursement market is rapidly growing, fueled by expanding health insurance coverage and government initiatives like Ayushman Bharat. With increasing private sector participation, the country is evolving its healthcare reimbursement models to improve accessibility and affordability. The rise of digital health infrastructure and telemedicine services is playing a crucial role in shaping reimbursement policies. These factors are making healthcare more accessible, addressing the needs of India’s vast population, and driving the market's ongoing development in both urban and rural areas.
- China- China’s market for healthcare reimbursement is driven by government reforms aimed at expanding insurance coverage and improving affordability. In July 2024, a National Library of Medicine study found that market competition significantly increased the success rate of cancer drug reimbursements. Drugs facing competition had an 84.6% success rate in gaining reimbursement, compared to 52.6% for non-competitive drugs. This competitive dynamic is enhancing access to cancer treatments, improving the affordability and effectiveness of healthcare in China, and strengthening the country’s reimbursement landscape.
Segmentation Analysis
The global healthcare reimbursement market is segmented into claim, payer, and service provider.
By Claim
The full reimbursement segment leads the market, offering complete coverage of medical expenses, thereby easing financial burdens on patients. This comprehensive coverage is particularly crucial for chronic diseases and critical care, where treatment costs are high. Both governments and private insurers are increasingly offering full reimbursement for essential treatments, which enhances healthcare accessibility and ensures that patients receive necessary care without significant out-of-pocket expenses.
By Payer
Public payers dominate the global market, holding the largest market share due to their extensive funding for essential medical services. Government-backed reimbursement policies, including universal health coverage and national insurance schemes, improve access to healthcare for geriatric and low-income populations. This broad coverage strengthens the role of public payers, ensuring affordable healthcare and expanding access to necessary treatments across diverse patient demographics.
By Service Provider
Hospitals lead the market, holding the highest market share due to their comprehensive range of services, large patient volumes, and eligibility for extensive reimbursement policies. As the healthcare landscape shifts toward value-based care models and bundled payment programs, hospital reimbursements are further driven by an emphasis on patient outcomes and cost-effectiveness. These evolving models support hospitals in providing high-quality care while optimizing reimbursement processes.
Company Market Share
Key players in the industry are focusing on adopting a range of key business strategies, such as strategic collaborations, product approvals, acquisitions, and product launches, to strengthen their presence in the market. Moreover, they are investing in research and development to drive innovation and enhance product offerings.
Care Health Insurance Ltd: An Emerging Player in the Global Healthcare Reimbursement Market
Care Health Insurance Ltd. is a prominent health insurance provider that offers comprehensive coverage for individuals, families, and corporate groups. The company specializes in delivering cashless treatment options, seamless reimbursement claims, and innovative healthcare financing solutions. By focusing on customer-centric services, Care Health Insurance ensures easy access to quality healthcare, promoting both financial protection and timely medical care.
Recent developments by Care Health Insurance Ltd:
- In January 2025, Care Health Insurance launched Ultimate Care, a comprehensive health insurance plan offering extensive benefits and incentives for maintaining good health. The plan features a MoneyBack benefit, refunding the first year’s base premium after every five claim-free years, and a Loyalty Boost, adding an extra sum insured after seven claim-free years.
List of Key and Emerging Players in Healthcare Reimbursement Market
- UNITEDHEALTH GROUP
- Aviva
- Allianz Care
- CVS Health
- BNP Paribas
- Aetna Inc.
- Nippon Life Insurance Company
- Cigna Healthcare
- Blue Cross Blue Shield Association
- Prudential Hong Kong Limited
- Care Health Insurance Ltd.
- Niva Bupa
- Centene Corporation
- Reliance General Insurance
- Agile Health

to learn more about this report Download Market Share
Recent Developments
- September 2024 – Cigna Healthcare, the health benefits division of The Cigna Group, introduced an E-Treatment option via MDLIVE by Evernorth. This service allows customers to receive urgent care for common conditions like allergies, infections, and respiratory illnesses without phone or video consultations. Through the MDLIVE portal, users can submit a virtual clinical interview and receive diagnoses and personalized treatment plans within an hour, enhancing convenience and accessibility in digital healthcare reimbursement.
Analyst Opinion
As per our analyst, the global healthcare reimbursement market is poised for substantial growth, driven by evolving regulatory frameworks, an increasing burden of chronic diseases, and the rapid advancement of digital health solutions. Governments and insurers are placing a strong emphasis on value-based care models, which prioritize patient outcomes over the volume of services provided.
Moreover, reimbursement for remote patient monitoring (RPM) and personalized treatments is expanding, improving access to care while managing costs. However, despite these positive developments, challenges remain, including the complexity of reimbursement policies, the slow pace of regulatory adaptations in certain regions, and the limited coverage of advanced treatments such as gene therapy and precision medicine.
Despite these hurdles, the market continues to thrive, especially in emerging economies across Asia-Pacific and Latin America, where rapid healthcare infrastructure development, increasing insurance penetration, and rising demand for affordable healthcare solutions are creating new opportunities. These regions are expected to be key drivers in future growth as both public and private sectors work to improve healthcare access and affordability.
Report Scope
| Report Metric | Details |
|---|---|
| Market Size in 2024 | USD 28.69 Billion |
| Market Size in 2025 | USD 35.55 Billion |
| Market Size in 2033 | USD 90.43 Billion |
| CAGR | 12.43% (2025-2033) |
| Base Year for Estimation | 2024 |
| Historical Data | 2021-2023 |
| Forecast Period | 2025-2033 |
| Report Coverage | Revenue Forecast, Competitive Landscape, Growth Factors, Environment & Regulatory Landscape and Trends |
| Segments Covered | By Claim, By Payer, By Service Provider |
| Geographies Covered | North America, Europe, APAC, Middle East and Africa, LATAM |
| Countries Covered | US, Canada, UK, Germany, France, Spain, Italy, Russia, Nordic, Benelux, China, Korea, Japan, India, Australia, Taiwan, South East Asia, UAE, Turkey, Saudi Arabia, South Africa, Egypt, Nigeria, Brazil, Mexico, Argentina, Chile, Colombia |
to learn more about this report Download Free Sample Report
Healthcare Reimbursement Market Segments
By Claim
- Full Reimbursement
- Partial Reimbursement
By Payer
- Public Payers
- Private Payers
By Service Provider
- Hospitals
- Specialty Clinics
- Diagnostics Laboratory
- Ambulatory Surgery Center
By Region
- North America
- Europe
- APAC
- Middle East and Africa
- LATAM
Frequently Asked Questions (FAQs)
Debashree Bora
Healthcare Lead
Debashree Bora is a Healthcare Lead with over 7 years of industry experience, specializing in Healthcare IT. She provides comprehensive market insights on digital health, electronic medical records, telehealth, and healthcare analytics. Debashree’s research supports organizations in adopting technology-driven healthcare solutions, improving patient care, and achieving operational efficiency in a rapidly transforming healthcare ecosystem.










































