Medical Billing Software Market Size, Share & Trends Analysis Report By Component (Solution, Services), By Type (Professional billing, Institutional billing), By End-User (Multi-specialty hospitals, Super specialty hospitals, Clinics, Pharma and medical), By Deployment (On-premises, Cloud-based) and By Region (North America, Europe, APAC, Middle East and Africa, LATAM) Forecasts, 2025-2033
Medical Billing Software Market Size
The global medical billing software market size was worth USD 15.34 billion in 2024 and is estimated to reach an expected value of USD 16.95 billion in 2025 to USD 37.68 billion by 2033, growing at a CAGR of 10.5% during the forecast period (2025-2033).
Medical Billing Software is a healthcare technology solution that automates the billing and revenue cycle management process for hospitals, clinics, and private practices. It enables healthcare providers to efficiently generate invoices, process insurance claims, track payments, and manage patient billing records. These systems often integrate with electronic health records (EHR) and practice management software to ensure seamless data exchange. By reducing manual paperwork, minimizing errors, and ensuring regulatory compliance (such as HIPAA in the U.S.), medical billing software helps healthcare facilities improve cash flow and streamline administrative workflows.
The growth in the global market has been tremendous in the last few years, mainly due to the increasing complexity of healthcare billing and the high cost of healthcare. More advanced technology such as artificial intelligence, machine learning, and cloud-based solutions help further accelerate growth in a way that has enhanced the accuracy of billing, reduced errors, and streamlined processes. One of the key trends in this area is integrating such software with EHRs and practice management systems, thus ensuring smooth data sharing and better operations. Telemedicine and remote healthcare have also increased the demand for web-based and cloud-based software, allowing providers to handle billing tasks from anywhere.
The below shows a sharp rise in diabetic cases, increasing from 101 in 2021 to 212 in 2022. This growth highlights potential health concerns, requiring further investigation into lifestyle, awareness, or environmental factors to manage and prevent diabetes effectively.
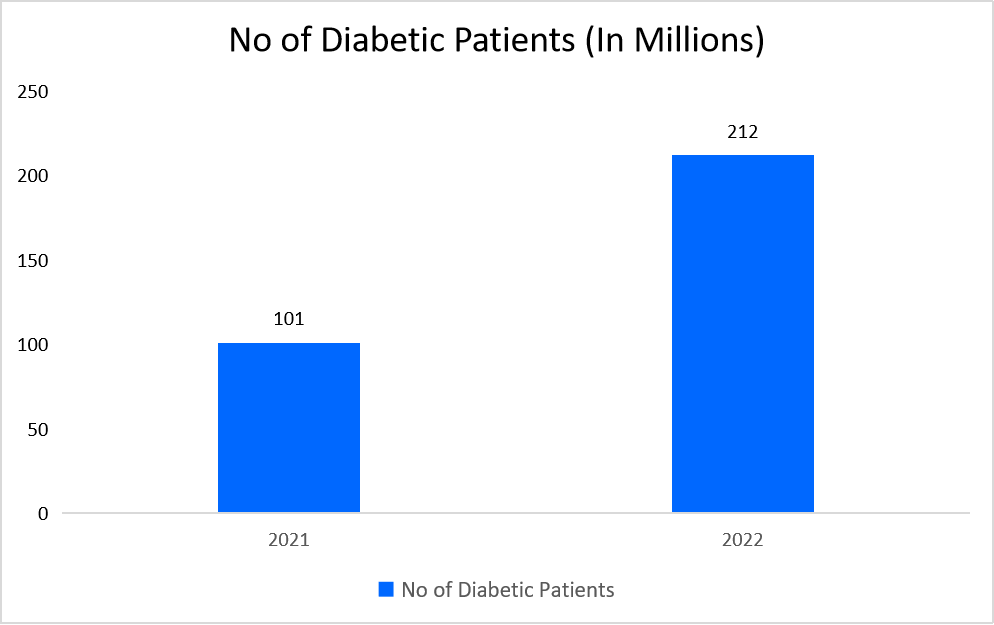
Source: Straits Research
Latest Market Trend
Rising Demand for Hcit Solutions
Healthcare information technologies are increasingly important to the demand for such software. HCIT solutions include advanced billing software, leading healthcare providers to obtain efficiency, reduce administrative activities, and provide appropriate and accurate billing and adherence. With the advance in digitization of healthcare systems, many healthcare providers are searching for integrated solutions.
- For instance, Waterbury Hospital adopted Cerner's Electronic Health Record (EHR) system coupled with TigerText's communication solution, saving more than USD 2,200 per patient. The integration also allowed for easier coordination among care providers, minimizing errors and, in turn, enhancing patient care, showing concrete advantages of embracing HCIT.
Furthermore, the increasing medical treatment costs are one of the significant trends influencing the market. Providers require strong billing solutions for complex pricing structures, accurate claims, and optimized revenue cycle management as healthcare costs rise. Such systems help streamline the billing process, reduce errors, and ensure financial sustainability for healthcare facilities.
Market Summary
| Market Metric | Details & Data (2024-2033) |
|---|---|
| 2024 Market Valuation | USD 15.34 Billion |
| Estimated 2025 Value | USD 16.95 Billion |
| Projected 2033 Value | USD 37.68 Billion |
| CAGR (2025-2033) | 10.5% |
| Dominant Region | North America |
| Fastest Growing Region | Europe |
| Key Market Players | Kareo, Inc., WebPT, Inc., athenahealth, ADT, Cognizant |

to learn more about this report Download Free Sample Report
Medical Billing Software Market Growth Factor
Growing Numbers of Patients
The demand for efficient and automated medical billing software is surging with the global rise in patient numbers, driven by an aging population and an increasing prevalence of chronic diseases. Hospitals, clinics, and other healthcare providers require seamless billing solutions to handle large patient volumes while complying with evolving regulatory standards. As healthcare systems become more complex, manual billing processes become inefficient, leading to an increasing reliance on advanced software for accurate claims processing and revenue cycle management.
- For instance, in the United States, the prevalence of chronic diseases continues to rise steadily. According to the Centers for Disease Control and Prevention (CDC), 51.8% of U.S. adults had at least one chronic condition, while 27.2% had multiple chronic conditions.
With the growing burden of chronic illnesses such as diabetes, cardiovascular diseases, and respiratory conditions, healthcare organizations are pressured to adopt technology-driven billing solutions to streamline reimbursement processes, reduce errors, and enhance financial performance. Additionally, government initiatives encouraging digital healthcare adoption further propel the market's growth.
Restraining Factor
High Cost of Deployment
Advanced medical billing systems require significant initial investments, which include software licensing fees, infrastructure setup, customization, and integration with existing healthcare IT systems. The ongoing costs associated with software maintenance, system updates, cybersecurity, and employee training further add to the financial burden. Small and medium-sized healthcare providers often find these costs prohibitive, making it challenging to implement robust solutions.
- For instance, Magrabi Hospitals in Saudi Arabia faced significant financial challenges when implementing a Health Information System (HIS) with medical billing functionality. Interoperability across departments requires substantial investments in new technology, process reengineering, and multi-phase deployment, highlighting healthcare organizations' substantial financial barriers.
Furthermore, concerns over data security, compliance with international regulations (such as HIPAA and GDPR), and vendor lock-in further hinder the widespread adoption of medical software in cost-sensitive markets.
Market Opportunity
Technology Advancements Solutions
Innovations in medical billing software, particularly AI-driven automation, cloud-based platforms, and blockchain integration, present substantial growth opportunities. These technologies enhance accuracy, reduce administrative burdens, minimize human errors, and improve efficiency. Moreover, advancing interoperability standards enables seamless integration with Electronic Health Records (EHRs), improving workflow cohesion and healthcare coordination.
- For instance, in 2023, Cedar, a healthcare financial platform, leveraged machine learning (ML) algorithms to optimize billing processes. This resulted in a 30% improvement in collection rates, significantly reducing errors and administrative time.
Additionally, AI-powered solutions enable predictive analytics for fraud detection and automated claims processing, which is expected to drive further adoption in the market. Cloud-based medical billing solutions are also gaining traction due to their scalability, lower infrastructure costs, and remote accessibility, making them particularly attractive to small and mid-sized healthcare providers.
Regional Insights
North America is the dominant global medical billing software market region because of several key factors. The area has an established healthcare infrastructure that has generally welcomed advanced technologies; in this regard, cloud-based systems do come into consideration. With a fragmented system involving many private insurers and government programs, the U.S. healthcare system is highly demanding, further needing medical billing solutions with expertise in navigating complex billing and reimbursement processes.
- For instance, eClinicalWorks is the most extensive cloud-based EHR system in the United States. It offers features for managing patient records and running medical practices. More than 110,000 healthcare facilities use this system, helping doctors and medical providers give great care while efficiently managing billing.
United States Market
The U.S. is the largest market for medical billing software, driven by stringent regulatory compliance requirements (HIPAA), EHR adoption, and AI-powered automation. Key players such as Epic Systems, Cerner, McKesson, and GE Healthcare are investing in cloud-based solutions and fraud detection algorithms to improve claim processing and reduce reimbursement delays.
Canada Market
The Canadian market, defined by its publicly funded healthcare system, focuses on efficiency and interoperability. TELUS Health, a leading healthcare IT provider, offers EHR and billing software solutions, improving claims management and financial transparency.
Asia Pacific Market
Asia-Pacific is growing rapidly in the global medical billing software market for several reasons. The region is experiencing huge improvements in healthcare, especially in developing countries, which need better solutions to handle the complexity of medical billing as their healthcare systems improve. New technologies, especially artificial intelligence, are changing how medical billing works by automating tasks, making it more accurate, and simplifying the process, which makes everything run more smoothly.
- For instance, according to a joint report by Bain & Co and APACMed (Asia Pacific Medical Technology Association), in partnership with the Singapore Economic Development Board, artificial intelligence will be a game-changer in the Asia-Pacific market in the long term. This innovation promises to streamline billing processes, improve accuracy, and enhance efficiency across the region's healthcare sector.
China Market
China’s rapid market expansion is fueled by government-led initiatives to modernize healthcare infrastructure and digitize medical billing. Tencent, a leading tech firm, offers electronic medical records (EMRs) and AI-driven billing solutions, accelerating healthcare digital transformation in China.
India Market
With increasing healthcare expenditures and a push towards digitalization, the market is booming. Sathguru Management Consultants provides market research and strategic guidance for healthcare IT adoption, promoting the expansion of digital billing solutions.
Japan Market
With a rapidly aging population and a high demand for efficient health services, the country embraces AI-driven billing solutions. Fujitsu, a Japanese technology giant, offers comprehensive healthcare IT solutions, including electronic medical records and automated billing platforms.
Germany Market
A well-established healthcare system with stringent data privacy laws (GDPR) supports adopting high-quality, secure billing solutions. CompuGroup Medical, a leading German firm, provides EHR and practice management software with built-in billing automation.
United Kingdom Market
The NHS drives the UK medical billing software market, focusing on cost reduction, care improvement, and digital transformation. EMIS Health provides advanced EHR and billing software solutions, improving hospital revenue cycles and patient management efficiency.
Brazil Market
An emerging market with increased healthcare spending and a growing middle class is boosting demand for medical billing software. TOTVS, a Brazilian IT solutions provider, develops healthcare-focused business management software, enabling streamlined revenue cycle management.
Billing Type Insights
Institutional Billing holds the most significant revenue in the market. This is because the segment will be essential for handling billing processes by large healthcare institutions such as hospitals and medical centers. Institutional billing usually involves complex processes due to the high number of claims and the range of services these institutions provide, hence the key revenue area in the medical billing landscape.
Deployment Mode Insights
The web-based segment is dominant and has the largest revenue share in the global market. The reason for their high preference is the accessibility of these solutions from any location with an internet connection and ease of integration with other software systems. The solutions offer improved scalability, flexibility, and security, key drivers behind their widespread adoption in the healthcare industry.
End-Use Insights
The Healthcare Providers segment dominates the market. Hospitals, clinics, and physician practices widely use medical billing software for efficiently handling accurate and timely billing, compliance with regulatory requirements, and patient data management. Healthcare providers form the majority of the market, handling most patient billing and payment transactions that are fundamental to the operation and finance of these health service providers.
Company Market Share
Key market players are investing in advanced medical billing software technologies and pursuing strategies such as collaborations, acquisitions, and partnerships to enhance their products and expand their market presence.
Oracle: An Emerging Player in the Medical Billing Software Market
Oracle is an emerging market player because of its strong technological foundation and innovative solutions. This company has profound knowledge of database management systems and cloud technology. Such expertise helps it deliver robust, scalable, and secure billing solutions for the different needs of healthcare organizations. Oracle's solutions are highly interoperable, meaning that they easily interface with EHRs and other healthcare systems, streamlining workflow and increasing data accuracy. Oracle emphasizes data security and regulatory compliance, such as HIPAA standards.
Recent Developments:
- In October 2024, Oracle announced the general availability of Oracle Health Clinical Data Exchange, a cloud-based solution that simplifies medical claims processing. Built on Oracle Cloud Infrastructure, it replaces manual record transmission with secure, automated data exchange, reducing administrative costs and accelerating claims processing and approvals.
List of Key and Emerging Players in Medical Billing Software Market
- Kareo, Inc.
- WebPT, Inc.
- athenahealth
- ADT
- Cognizant
- Epic Systems Corporation.
- GeBBS
- Healthray
- DrChrono (EverHealth Solutions Inc.)
- AGS Health
- Oracle
Recent Developments
- March 2024- DocStation and CPSEN joined forces to help pharmacies in provider status states: Minnesota, Texas, California, New York, Pennsylvania, Ohio, Tennessee, and Washington. They will offer guidance and educational support to the pharmacies to navigate the process of getting reimbursed for their services
- December 2024- Expert Medical Billing launched its Strategic Partnership Program, enabling healthcare consultants and startup advisors to enhance service offerings and create new revenue streams by integrating Expert Medical Billing's proven approach into their operations for long-term success.
Analyst Opinion
As per our analyst, the global medical billing software market is transforming significantly due to the rising complexity of healthcare revenue cycle management (RCM), widespread EHR adoption, and the shift towards value-based care models. As healthcare providers focus on improving accuracy, financial transparency, and regulatory compliance, demand for AI-powered, cloud-based, and automated billing solutions will continue to rise. The increasing adoption of cloud-based billing software is a major driver, offering scalability, cost-effectiveness, and seamless integration with existing healthcare systems.
Furthermore, strategic collaborations between tech firms and healthcare providers drive the next wave of billing innovation, making the software more affordable, accessible, and efficient across diverse healthcare settings. With continuous AI, blockchain, and automation improvements, the market is poised for sustained growth, offering enhanced revenue cycle management solutions for healthcare providers worldwide.
Report Scope
| Report Metric | Details |
|---|---|
| Market Size in 2024 | USD 15.34 Billion |
| Market Size in 2025 | USD 16.95 Billion |
| Market Size in 2033 | USD 37.68 Billion |
| CAGR | 10.5% (2025-2033) |
| Base Year for Estimation | 2024 |
| Historical Data | 2021-2023 |
| Forecast Period | 2025-2033 |
| Report Coverage | Revenue Forecast, Competitive Landscape, Growth Factors, Environment & Regulatory Landscape and Trends |
| Segments Covered | By Billing Type, By Deployment Mode, By End-use |
| Geographies Covered | North America, Europe, APAC, Middle East and Africa, LATAM |
| Countries Covered | US, Canada, UK, Germany, France, Spain, Italy, Russia, Nordic, Benelux, China, Korea, Japan, India, Australia, Taiwan, South East Asia, UAE, Turkey, Saudi Arabia, South Africa, Egypt, Nigeria, Brazil, Mexico, Argentina, Chile, Colombia |
to learn more about this report Download Free Sample Report
Medical Billing Software Market Segments
By Billing Type
- Professional Billing
- Institutional Billing
By Deployment Mode
- On-Premises
- Web-Based
- Cloud-Based
By End-use
- Healthcare Providers
- Healthcare Payers
- Others
By Region
- North America
- Europe
- APAC
- Middle East and Africa
- LATAM
Frequently Asked Questions (FAQs)
Debashree Bora
Healthcare Lead
Debashree Bora is a Healthcare Lead with over 7 years of industry experience, specializing in Healthcare IT. She provides comprehensive market insights on digital health, electronic medical records, telehealth, and healthcare analytics. Debashree’s research supports organizations in adopting technology-driven healthcare solutions, improving patient care, and achieving operational efficiency in a rapidly transforming healthcare ecosystem.










































