Skin Perfusion Pressure Testing Devices Market Size, Share & Trends Analysis Report By Product Type (Laser Doppler SPP Testing Devices, Photoplethysmography (PPG) SPP Testing Devices, Ultrasound Doppler SPP Testing Devices, Hybrid Multi-Function SPP Monitoring Systems), By Modality (Portable/Handheld Devices, Standalone Desktop Units, Integrated Bedside Monitoring Systems), By Application (Peripheral Arterial Disease (PAD) Diagnosis, Chronic Limb-Threatening Ischemia Assessment, Diabetic Foot Ulcer Management, Preoperative Surgical Evaluation, Postoperative Blood Flow Monitoring), By Distribution Channel (Direct Sales to Hospitals and Clinics, Medical Device Distributors, Online Medical Equipment Platforms, Tenders and Institutional Supply Contracts), By End-User (Hospitals & Specialty Clinics, Vascular and Wound Care Centres, Ambulatory Surgical Centres (ASCs), Home Healthcare Providers, Academic and Research Institutions) and By Region (North America, Europe, APAC, Middle East and Africa, LATAM) Forecasts, 2025-2033
Skin Perfusion Pressure Testing Devices Market Size
The global skin perfusion pressure (SPP) testing devices market size was valued at USD 387.2 million in 2024 and is projected to grow from USD 411.6 million in 2025 to USD 671.0 million by 2033, expanding at a CAGR of 6.3% during the forecast period (2025-2033).
The global skin perfusion pressure (SPP) testing devices market is experiencing steady growth, driven by the increasing incidence of chronic wounds, peripheral artery disease (PAD), and diabetes-related complications. SPP testing devices used to evaluate microcirculatory blood flow and predict wound healing capacity are gaining widespread adoption across hospitals, wound care centres, and vascular clinics due to their non-invasive design and greater accuracy than traditional methods like the ankle-brachial index (ABI). Their use is accelerating amid growing emphasis on early detection of limb ischemia and personalised revascularisation strategies, particularly for diabetic and elderly patients.
Current Market Trend
Integrated Perfusion Monitoring Enhances Vascular Care
The skin perfusion pressure (SPP) testing devices market is driven by the move toward integrated diagnostic platforms that combine key vascular parameters, such as compartment pressure (CP), diastolic blood pressure (DBP), and perfusion pressure (ΔP), into a single, portable system. With rising demand for non-invasive, real-time diagnostic tools, especially in trauma care, diabetic foot ulcer (DFU) management, and critical limb ischemia (CLI) assessment, manufacturers are introducing multifunctional devices that eliminate the need for separate instruments while enhancing diagnostic precision and patient outcomes.
- For example, in March 2025, MY01 received FDA clearance for its next-generation perfusion monitoring feature, which integrates CP, DBP, and ΔP readings into a single device.
The integration of multi-parameter functionality is a driving force in reshaping vascular assessment practices and broadening access to critical diagnostic information in both hospital and community-based care environments.
Market Summary
| Market Metric | Details & Data (2024-2033) |
|---|---|
| 2024 Market Valuation | USD 387.2 Million |
| Estimated 2025 Value | USD 411.6 Million |
| Projected 2033 Value | USD 671.0 Million |
| CAGR (2025-2033) | 6.3% |
| Dominant Region | North America |
| Fastest Growing Region | Asia Pacific |
| Key Market Players | Perimed AB, Moor Instruments Ltd., LD Technology, Vasamed Inc., Transonic Systems Inc. |

to learn more about this report Download Free Sample Report
Skin Perfusion Pressure Testing Devices Market Driver
Telehealth Expansion and Ai Integration
A significant driver of the skin perfusion pressure testing devices market in 2025 is the healthcare sector’s shift toward AI-enabled diagnostics and remote monitoring, which is driving demand for portable, connected SPP devices across outpatient and decentralised care settings. With the rising burden of diabetes-related vascular complications and chronic wounds, point-of-care solutions for early perfusion assessment are becoming central to preventative care models.
- For instance, in January 2025, a Langate review of healthcare technology trends highlighted that AI-enabled diagnostics and telehealth expansion remain central strategies for hospitals and clinics, reshaping patient care pathways and accelerating the shift toward decentralised, data-driven models. This digital push drives the adoption of advanced analytics tools that support non-invasive vascular assessments, including skin perfusion pressure (SPP) testing.
The growth of telehealth infrastructure and clinical demand for fast, quantitative diagnostics is encouraging providers to deploy compact SPP devices in non-traditional settings. Manufacturers developing AI-enhanced, cloud-connected models are well-positioned to capture rising market interest.
Market Restraining Factor
Lack of Standardised Diagnostic Protocols Limits Clinical Integration
The absence of universally accepted clinical guidelines and diagnostic thresholds for interpreting SPP results restricts the market. Unlike more established diagnostics such as the ankle-brachial index (ABI), SPP testing lacks global consensus on cutoff values for ischemia or perfusion adequacy. For instance, some vascular clinics interpret an SPP of <30 mmHg as critical ischemia, while others use different benchmarks depending on patient comorbidities, wound depth, or device calibration. This variability can lead to discrepancies in diagnosis, delayed interventions, or redundant testing with other modalities.
Furthermore, the diversity of device technologies, ranging from laser Doppler systems to photoplethysmography-based tools, may yield different readings under the same clinical conditions. The absence of calibration standards and cross-platform validation hampers clinical confidence and slows device adoption, particularly in hospitals prioritising evidence-based practice.
Market Opportunity
Advanced Vascular Imaging Technique Unlocks Enhanced Diagnostic Accuracy
A promising breakthrough emerged with developing a novel imaging technique that combines Laser Speckle Contrast Imaging (LSCI) with advanced data processing methods, specifically principal component analysis and entropy filtering. This approach significantly enhances image contrast, minimises interference from static tissue scatterers, and improves sensitivity to subtle changes in blood flow velocity. These advancements are critical in non-invasive vascular assessment, enabling clinicians to detect and monitor vascular abnormalities with greater accuracy and efficiency.
- For instance, in January 2025, researchers published their findings in Frontiers of Optoelectronics, demonstrating that the integrated technique provides clearer and more precise blood flow measurements essential for diagnosing vascular diseases. The method’s ability to isolate dynamic blood flow signals from static tissue noise sets a new standard for image clarity, crucial for assessing microvascular health.
Beyond improving diagnostic accuracy, this technology opens new avenues for clinical applications across chronic wound care, diabetes management, and other conditions where the microcirculatory function is key.
Regional Insights
North America's leadership in the SPP testing devices market is driven by its robust vascular diagnostics ecosystem and early adoption of microcirculation tools in clinical protocols. The region benefits from favorable reimbursement frameworks, physician training modules, and strong research support from clinical societies. North America also hosts several major SPP device manufacturers, facilitating quick access to upgrades, service contracts, and AI-driven software solutions. These elements collectively enable consistent technology adoption across care settings and ensure alignment with evolving standards in chronic wound management and peripheral artery disease (PAD) diagnostics.
U.s Skin Perfusion Pressure Testing Devices Market Trends
- The U.S. stands at the forefront of global SPP adoption due to its advanced clinical infrastructure, strong reimbursement landscape, and leadership in vascular research. Hospitals and specialized wound centres widely use SPP for diabetic foot management and ischemia risk stratification. Expanding reimbursement to include remote wound monitoring is promoting use in telehealth and home care environments. U.S. device manufacturers are pioneering AI-powered SPP solutions, combining real-time perfusion analytics with cloud-based reporting.
- Canada’s SPP testing devices market is growing steadily, supported by provincial health reforms emphasizing early PAD detection and limb preservation in chronic care. Government-backed reimbursement programs now support using SPP devices in diabetic foot clinics and long-term care facilities. Clinical adoption is particularly strong in urban health systems, where multidisciplinary vascular teams integrate SPP into wound care assessments and discharge planning. Additionally, national initiatives to reduce amputation rates among Indigenous and rural populations are spurring demand for portable and telemonitoring-compatible SPP units.
Asia-Pacific: Fastest-Growing Region
Asia-Pacific is the fastest-growing region in the SPP testing devices market, driven by a convergence of epidemiological need and healthcare modernisation. Rising diabetes prevalence, especially in countries like India and China, has spurred demand for early-stage PAD diagnostics to prevent limb complications. Japan and South Korea are advancing clinical integration of SPP into diabetic foot management protocols, supported by governmental guidelines. Additionally, expanding tertiary care facilities, digital health initiatives, and increased procurement budgets enable the rapid deployment of portable SPP units. The regional focus on decentralised care delivery makes Asia-Pacific a critical growth avenue for next-generation SPP innovations.
- Japan continues to lead in high-precision, compact SPP devices due to its ageing population and national focus on vascular diagnostics. Including SPP in diabetic foot guidelines has accelerated clinical use, particularly in tertiary hospitals and community care centres. Japan’s strength in medical electronics is enabling the development of mobile-compatible, lightweight SPP systems ideal for home monitoring and nurse-led wound care. Institutional partnerships between academia and device manufacturers are shaping innovations that align with Japan’s preventive care strategies and increasing demand for outpatient vascular assessment tools.
- India is evolving as a promising SPP testing devices market due to a sharp rise in diabetes-related complications and a growing focus on cost-effective diagnostic tools. Affordable, durable, and easy-to-use SPP devices tailored for regional health systems are being co-developed by local innovators and multinational firms. These models aim to serve under-resourced districts and primary care centres. Mobile health units equipped with SPP devices are also being piloted in rural areas under public-private initiatives. Integrating SPP into broader non-communicable disease management pathways could further accelerate market traction.
Europe: Significant Growth
Europe presents a mature, steadily expanding SPP testing devices market shaped by clinical validation, policy-backed healthcare reform, and aging populations. Preventive vascular diagnostics are a key regional priority, with countries such as Germany, the UK, and the Netherlands embedding SPP within limb preservation strategies and home-based wound care protocols. Moreover, hospital networks and specialist clinics across the continent are increasingly adopting portable SPP tools to reduce hospitalization and enhance ambulatory care. Europe’s harmonized regulatory environment and academic research infrastructure position it as a centre for SPP-related trials and policy-led innovation in vascular diagnostics.
- Germany plays a strategic role in Europe’s SPP ecosystem, leveraging its structured hospital network and proactive public health policies. Recent outpatient care reforms incentivize vascular clinics and private practices to adopt certified microcirculation tools. The presence of domestic medtech companies supports timely innovation and device customization. Additionally, German academic centres are leading clinical trials that evaluate SPP’s predictive accuracy for revascularisation outcomes. This evidence-driven approach reinforces clinical confidence and expands reimbursement pathways, further strengthening Germany’s position in Europe’s advanced vascular diagnostics segment.
- The UK represents a model for structured SPP deployment within national health systems. With NICE endorsing SPP for wound care and ischemia monitoring, specialised diabetic foot units and home care services increasingly use portable SPP systems for real-time perfusion tracking. National funding initiatives support technology rollout, particularly within preventive care and limb salvage programs. Cross-sector collaborations among the NHS, universities, and medtech suppliers enable outcome-based research and digital integration.
Product Type Insights
Laser Doppler-based SPP testing devices lead the global market owing to their unmatched precision in assessing microvascular blood flow. These devices utilise low-intensity laser beams that reflect off moving red blood cells, enabling clinicians to obtain real-time perfusion data during rest and post-occlusion phases. Their high diagnostic accuracy and non-invasive nature make them indispensable in outpatient wound care, vascular labs, and home-based clinical settings. The ease of use, compact design, and minimal patient discomfort have contributed to their growing adoption across various care environments, especially for managing chronic wounds and high-risk patients requiring frequent vascular assessments.
Modality Insights
Portable SPP devices are gaining traction due to their suitability for point-of-care diagnostics and decentralised healthcare delivery. These lightweight, battery-operated units provide flexibility for bedside assessments, remote clinics, and home care scenarios, eliminating reliance on large benchtop systems. Their role has expanded with the rise of telemedicine and mobile health services, particularly for elderly, diabetic, and post-operative patients. The convenience, speed, and versatility of portable models support early diagnosis of limb ischemia, enhancing preventive care and timely specialist referral. As healthcare systems move toward patient-centred models, portable SPP devices are becoming standard vascular triage and community-based care tools.
Application Insights
Chronic wound management is the fastest-growing application for SPP testing, driven by its effectiveness in evaluating tissue viability in conditions like diabetic foot ulcers, pressure sores, and venous leg ulcers. SPP measurements provide a reliable, quantitative indicator of local blood flow, guiding clinicians on treatment timing and modality, whether surgical debridement, compression therapy, or revascularisation. As wound complexity increases alongside the global diabetes burden, SPP testing is being adopted into advanced wound care protocols to optimise healing outcomes and reduce complications. Its utility in treatment planning makes it a critical diagnostic component across wound centers, burn units, and vascular outpatient services.
Distribution Channel Insights
Direct sales channels dominate the market due to the SPP testing devices' complex and technical nature, which requires training, software integration, and post-installation support. Manufacturers prefer engaging directly with hospitals, wound care centers, and vascular clinics to ensure proper device deployment and user proficiency. Many offer comprehensive sales packages to increase value and client retention, including consumables, calibration kits, and maintenance contracts. This direct approach enables customization, faster troubleshooting, and closer feedback loops, all essential for high-cost diagnostic systems. Direct sales will remain a preferred go-to-market strategy as SPP devices evolve with analytics platforms and connectivity features.
End-User Insights
Hospitals represent the primary end users of SPP testing devices, particularly within departments focused on vascular surgery, interventional radiology, and complex wound management. These institutions demand high diagnostic precision and favor integrated systems that align with electronic health records and clinical workflows. Multi-channel devices that support simultaneous testing at various sites enhance efficiency and documentation. Additionally, hospitals are under pressure to improve outcomes and reduce lower limb amputation rates, especially in diabetic populations. As a result, the clinical validation and reimbursement potential of SPP testing in North America, Japan, and parts of Europe are encouraging widespread hospital adoption as part of comprehensive vascular care.
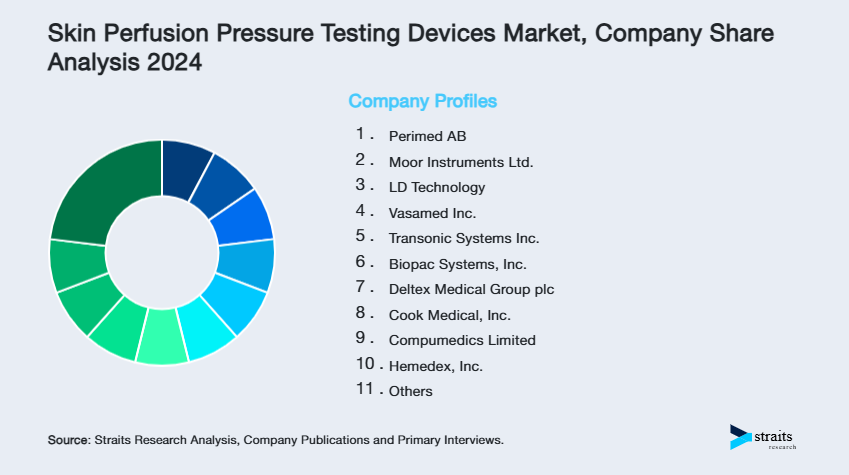
Company Market Share
The skin perfusion pressure (SPP) testing devices market remains moderately consolidated, with a few global and regional players dominating niche technology segments. Companies differentiate through proprietary vascular imaging technology, FDA-cleared platforms, and strong regional distribution alliances. Growth strategies increasingly focus on federal procurement, ambulatory care adoption, and expansion into limb salvage programs.
Perimed AB: Perimed AB is a well-established and respected leader in the skin perfusion pressure (SPP) testing devices market, and it is particularly renowned for its laser Doppler technology. With over 40 years of experience, they are a primary innovator and provider of non-invasive microcirculatory assessment tools. Their PeriFlux systems are widely used globally in wound care, diabetic foot clinics, and vascular diagnostics, making them a significant and trusted player.
- In 2024, Perimed AB signed a strategic partnership with Lovell Government Services, a U.S. federal contracting specialist. This collaboration enabled the deployment of Perimed’s laser-Doppler SPP systems across Veterans Affairs hospitals, Department of Defence clinics, and other federal healthcare sites. Lovell has secured multiple federal contracts, significantly enhancing Perimed’s access to institutional markets and expanding its footprint in government-funded wound care and vascular diagnostics.
List of Key and Emerging Players in Skin Perfusion Pressure Testing Devices Market
- Perimed AB
- Moor Instruments Ltd.
- LD Technology
- Vasamed Inc.
- Transonic Systems Inc.
- Biopac Systems, Inc.
- Deltex Medical Group plc
- Cook Medical, Inc.
- Compumedics Limited
- Hemedex, Inc.
- Elfi-Tech Ltd.
- Medstorm Innovation AS
- Kaneka Medix Corporation
- Finapres Medical Systems
to learn more about this report Download Market Share
Recent Developments
- April 2025– A significant study published in Clinical and Experimental Nephrology in April 2025 demonstrated that skin perfusion pressure (SPP), when measured at the initiation of hemodialysis (referred to as SPPₘᵢₙ), serves as a powerful prognostic indicator for patient outcomes over the course of one year. The research found that patients presenting with an SPP value below 60 mmHg at the start of dialysis faced considerably higher risks of mortality and cardiovascular complications within the first year of treatment.
- June 2025 – At the Japanese Society for Dialysis Therapy (JSDT) conference, researchers presented novel findings demonstrating that thermal far-infrared (FIR) therapy can significantly increase skin perfusion pressure (SPP) in limb blood flow assessments. Using advanced SPP sensors, they tracked perfusion changes in real time following FIR treatment in patients with dialysis access.
Report Scope
| Report Metric | Details |
|---|---|
| Market Size in 2024 | USD 387.2 Million |
| Market Size in 2025 | USD 411.6 Million |
| Market Size in 2033 | USD 671.0 Million |
| CAGR | 6.3% (2025-2033) |
| Base Year for Estimation | 2024 |
| Historical Data | 2021-2023 |
| Forecast Period | 2025-2033 |
| Report Coverage | Revenue Forecast, Competitive Landscape, Growth Factors, Environment & Regulatory Landscape and Trends |
| Segments Covered | By Product Type, By Modality, By Application, By Distribution Channel, By End-User |
| Geographies Covered | North America, Europe, APAC, Middle East and Africa, LATAM |
| Countries Covered | US, Canada, UK, Germany, France, Spain, Italy, Russia, Nordic, Benelux, China, Korea, Japan, India, Australia, Taiwan, South East Asia, UAE, Turkey, Saudi Arabia, South Africa, Egypt, Nigeria, Brazil, Mexico, Argentina, Chile, Colombia |
to learn more about this report Download Free Sample Report
Skin Perfusion Pressure Testing Devices Market Segments
By Product Type
- Laser Doppler SPP Testing Devices
- Photoplethysmography (PPG) SPP Testing Devices
- Ultrasound Doppler SPP Testing Devices
- Hybrid Multi-Function SPP Monitoring Systems
By Modality
- Portable/Handheld Devices
- Standalone Desktop Units
- Integrated Bedside Monitoring Systems
By Application
- Peripheral Arterial Disease (PAD) Diagnosis
- Chronic Limb-Threatening Ischemia Assessment
- Diabetic Foot Ulcer Management
- Preoperative Surgical Evaluation
- Postoperative Blood Flow Monitoring
By Distribution Channel
- Direct Sales to Hospitals and Clinics
- Medical Device Distributors
- Online Medical Equipment Platforms
- Tenders and Institutional Supply Contracts
By End-User
- Hospitals & Specialty Clinics
- Vascular and Wound Care Centres
- Ambulatory Surgical Centres (ASCs)
- Home Healthcare Providers
- Academic and Research Institutions
By Region
- North America
- Europe
- APAC
- Middle East and Africa
- LATAM
Frequently Asked Questions (FAQs)
Jay Mehta
Research Analyst
Jay Mehta is a Research Analyst with over 4 years of experience in the Medical Devices industry. His expertise spans market sizing, technology assessment, and competitive analysis. Jay’s research supports manufacturers, investors, and healthcare providers in understanding device innovations, regulatory landscapes, and emerging market opportunities worldwide.










































